Nicole Wolter, National Institute for Communicable Diseases
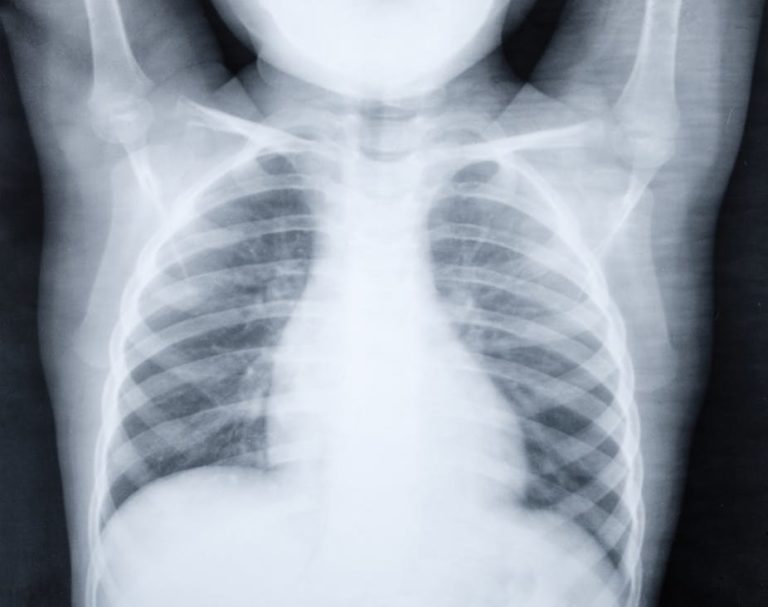
Pneumonia is a respiratory infection that affects the lungs. The viruses and bacteria that cause the disease are spread through airborne droplets from a cough or sneeze. An infection can cause the lungs to fill with pus and fluid, making breathing and oxygen intake difficult. And while anyone can get pneumonia, children with weakened immune systems or underlying illnesses are more susceptible. That’s why pneumonia kills more than a million children every year across the world.
There have been some critical advances in preventing and treating the disease. These include vaccines, antibiotics and providing supplemental oxygen. In 2009, South Africa became the first African country to include the pneumococcal conjugate vaccine in its routine infant immunisation programme. By 2012 an estimated 81% of one-year-old babies had received three doses of the vaccine.
South Africa has also reduced its pneumonia burden through the mass roll-out of antiretroviral therapy and the HIV prevention of mother-to-child transmission programme. This has made a difference because children born to HIV-infected mothers have a significantly increased risk of pneumonia disease and death.
But much work remains. In 2016 influenza and pneumonia were the second leading cause of death in children younger than five years in South Africa. That’s why we at the country’s National Institute for Communicable Diseases are monitoring key areas related to the cause and effects of pneumonia.
There is reason to be optimistic: a number of advances currently in development will almost certainly strengthen our artillery in the fight against pneumonia. Some of these are complicated and expensive, such as developing additional and more effective vaccines. But there are also many tools that don’t involve expensive, complicated medical interventions such as providing adequate nutrition, clean air and water.
There is an argument to be made for getting back to basics in a bid to tackle pneumonia. The answer to stopping children dying from preventable diseases may simply lie in basics such as reducing poverty and inequity.
Advances
As with any other disease, data is crucial when it comes to understanding and, ultimately, controlling pneumonia. At the institute, we examine what pneumonia-causing pathogen strains are circulating at any given time. We also keep a close eye on population groups at risk of infection and death (such as children) and monitor the effect that existing vaccines have on the disease.
All this data helps to detect increases in disease. This helps us to prepare rapid responses and work towards containment should an outbreak occur.
The information we collect can also help those who are trying to develop new pneumonia vaccines and improve current vaccine schedules. For instance, immunisation of women in their third trimester of pregnancy to provide protection to their babies in their first few months of life when they are most vulnerable.
In addition, vaccine candidates targeted against one of the viruses responsible for a significant proportion of childhood pneumonia – the respiratory syncytial virus (RSV) – are in the late stages of development.
Other advances are being made to improve pneumonia diagnosis. These include improved radiological methods, point-of-care tests which are used at or near patient care to speed up diagnosis, and the use of host biomarkers that examine the type of immune response a person develops to identify the cause of infection.
Back to basics
We know that malnutrition, indoor household air pollution, poverty, poor hygiene and sanitation all significantly increase a child’s risk of infection and death.
In South Africa, about 30,3 million people were living below the poverty line in 2015. Two-thirds of children younger than 18 years were living in poverty.
It is critical to provide children with basic human needs like adequate nourishment, access to clean water and air, and equitable access to vaccines and basic healthcare.
The costs associated with improving children’s living conditions must be evaluated against the high costs associated with the clinical management of childhood pneumonia. The residual burden of pneumonia can be reduced by prioritising child health through simple interventions. These include improving living conditions and accessibility to affordable medication, vaccines and care.![]()
Nicole Wolter, Principal Medical Scientist, National Institute for Communicable Diseases
This article is republished from The Conversation under a Creative Commons license. Read the original article.