
Shutterstock
Nazir Ismail, National Institute for Communicable Diseases
The world marks World Tuberculosis (TB) Day on March 24 every year. Most people assume that TB only affects the lungs – but the disease can also attack other organs. The Conversation Africa’s Ina Skosana spoke to Professor Nazir Ismail to find out more. Professor Ismail works and conducts his research in South Africa, one of the world’s TB hot spots.
What parts of the body does TB affect?
TB most commonly affects the lungs – what’s known as the body’s pulmonary system. But it affects other organs too, what’s known as extrapulmonary TB.
Other organs that can be affected include the lining covering the lungs (pleural TB); the central nervous system (TB meningitis); bone and joints (musculoskeletal system); lymph nodes; abdomen – where the liver, spleen and the intestines can be affected (abdominal TB); kidney and bladder (urogenital TB); and blood.
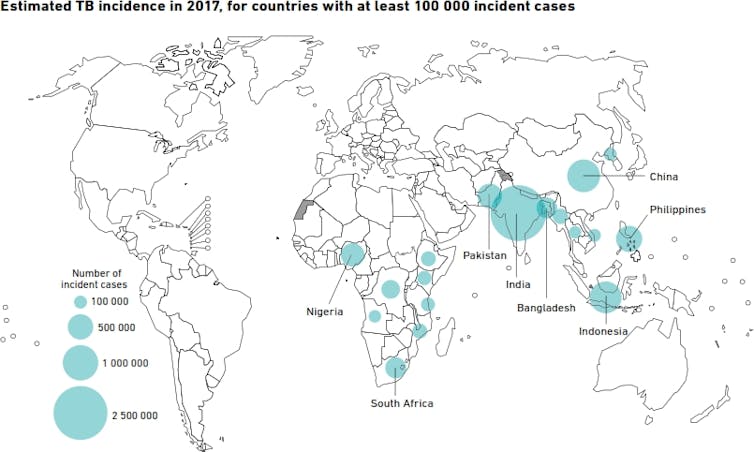
WHO Global TB report 2018
A study conducted in Johannesburg showed that the most common sites of extra pulmonary TB were the pleura (39.1%), lymph nodes (31.0%), blood (21.8%), central nervous system (7.3%), and abdomen (2.9%).
Another study conducted in the KwaZulu-Natal province also showed pleural TB to be the most common form of extra pulmonary TB (36% of patients).
How common is this form of TB? What causes it?
According to the World Health Organisation’s most recent TB report, extrapulmonary TB accounted for 14% of TB cases recorded globally in 2017. Across the African continent, extrapulmonary TB accounted for 16% of the 1 323 450 cases recorded. In South Africa it accounts for 11% of all TB cases reported.
Importantly – unlike pulmonary TB, which is spread through the air from person to person – extrapulmonary TB is not infectious.
A key risk factor for developing extrapulmonary TB is a compromised immune system which is why it is more common in patients infected with HIV. It can also occur in people with diabetes, cancer, low body weight and chronic kidney disease. Smoking and the use of drugs that can suppress the immune system also increase the risk of extrapulmonary TB.
Though the risk factors differ, all types of TB develop in the same way. TB infection occurs when a person inhales droplet particles containing the TB bacterium. Once inhaled, the bacteria then heads for the lungs. If the immune system is fully functional, several mechanisms are put in place by the body’s response to the foreign agent to contain the bacteria. The end result is usually a walled off “granuloma”, preventing the TB bacteria from multiplying and making the person ill.
In some patients, the TB escapes to another part of the body before the lungs can wall it off. In healthy people with strong immune systems, other organs or systems will put up a “barrier” that’s similar to the lung’s granuloma.
But if this defence mechanism fails, the bacteria multiply and cause disease in that specific organ system. This is called primary TB and is usually seen in young children.
Sometimes, a person can successfully wall off TB when they are healthy. But as their immune system weakens – because of old age, or conditions like HIV and diabetes – the wall can break down. If that happens, the bacteria can multiply and lead to active disease.
How is extrapulmonary TB diagnosed and treated?
Clinicians find it challenging to diagnose extrapulmonary TB. This is because the patient doesn’t present with the typical signs and symptoms of pulmonary TB – chronic cough, fever, loss of weight and night sweats. In some cases, the presenting signs and symptoms can be very vague and can mimic other conditions. All this means the clinician must have a strong suspicion that their patient has extrapulmonary TB to even start seeking this diagnosis.
Investigations include X-rays, CT scans or MRIs and sending appropriate specimens to the laboratory to detect the TB bacterium. The type of specimen that should be sent depends on the organ system involved. For example, in the case of lymph node TB, a biopsy (tissue specimen) of the lymph node should be sent to the laboratory; in the case of pleural TB, pleural fluid should be sent for testing.
It is important to note that in certain instances, even though the laboratory result might be negative, the clinician may still opt to treat for tuberculosis based on the high clinical suspicion, constellation of clinical signs and symptoms; and adjunct special investigations (biopsy, CT scans).
The drugs used to treat extrapulmonary TB are the same as those used for the treatment of pulmonary TB. The only difference is that the duration of treatment for extrapulmonary TB is longer and depends on the organ system involved. Most extrapulmonary TB is treated for nine months but can sometimes be longer. Treatment is taken orally and is a combination tablet that is dosed based on a person’s weight. Hospital admission is not required for treatment unless the patient is severely ill. Patients can continue to take their medication at home.
How does a person know they’ve got it?
The presentation of extrapulmonary TB depends on which organ is involved. An example is lymph node TB on a person’s neck which would present as a noticeable growth or lump. There are multiple causes for such a growth, one of which is TB, which the doctor would know to investigate. Thus seeking medical advice early when you are unwell is an important starting point.![]()
Nazir Ismail, Head of the Centre for Tuberculosis, National Institute for Communicable Diseases
This article is republished from The Conversation under a Creative Commons license. Read the original article.





