Rabies Updates
Rabies is a zoonotic, vaccine-preventable viral disease that causes damage to the brain and spinal cord in infected animals and humans. A zoonotic disease is a disease that can be transmitted between animals and humans. Rabies is nearly 100% fatal once symptoms appear.
The rabies virus is spread to humans and other animals through contact with saliva of infected animals. Bites or scratches or licks to wounds, grazes, broken skin, or to the lining of the mouth and nose are examples of unsafe contact. Human-to-human transmission is not known apart from rare cases associated with organ transplantation. Most human rabies cases in South Africa are linked to rabid domestic dogs.
As in animals, rabies in humans can present in the furious (hyperactive/agitated) or paralytic (dumb) forms. The common signs and symptoms of rabies include discomfort or pain at the site of the (previous) wound, fever, headache nausea and vomiting. This rapidly progress to signs of neurological dysfunction, which may include changed behavior, anxiety, confusion, and agitation.
People with rabies can also display hypersalivation, aerophobia (fear of air) and hydrophobia (fear of water). Some people may have localized weakness, paralytic syndromes, which eventually progress to coma and death. Rabies is a fatal infection in humans and only exceptionally rare cases of survival have been reported to date.
In South Africa, mostly domestic dogs are diagnosed with rabies. Other animals may also be infected with the virus, including domestic livestock (such as cattle and sheep) and wildlife (such as jackal). Rabies is not typically reported from small rodents such as mice and rats. It is also not reported from birds or reptiles. There are no rabies viruses reported in bats in South Africa. There are however, “rabieslike” viruses reported rarely in some species of bats and have related to two human rabies cases in South Africa in the past 40 years.
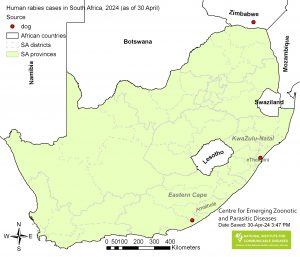
Human rabies is rare, but still reported in South Africa. Typically, 5 – 10 cases of human rabies are laboratory confirmed per year. During the first quarter of 2024 (1 January to 30 April), 3 cases of human rabies were reported in South Africa. These cases were reported from the eThekwini Municipality, KZN and the Ngqushwa Municipality, Amathole district, EC.
Recent Updates
FAQ
Most frequent questions and answers about Rabies
In the past ten years, rabies has been reported mostly in domestic dogs from areas in the KwaZuluNatal, Eastern Cape and Limpopo provinces. It is important to note, that outbreaks of rabies in domestic dogs may however occur in any area of South Africa where unvaccinated domestic dogs present a susceptible population for transmission of the virus. Rabies is reported from mongoose,
black-backed jackal, and bat-eared fox in other areas of South Africa.
Sporadic cases involving other domestic and wildlife species are also reported from time-to-time. Human rabies cases are usually reported from areas where domestic dog rabies is found.
If no post-exposure prophylaxis is given, an infected person may start experiencing symptoms 1 to 3 months after exposure. In rare cases, symptoms can develop after 14 weeks or after more than six months, following an exposure. Very short incubation periods have been rarely recorded in cases with facial wounds or wounds in other highly innervated areas of the body.
Rabies can be controlled by vaccinating dogs (and cats) and thereby protecting those animals and also decreasing the risk of human exposure to the virus. All domestic dogs and cats should be vaccinated against rabies from 12 weeks of age and again 12 months later, and then every 1-3 years.
Once exposure has occurred, rabies infection in humans can be prevented by prompt administration of rabies post-exposure prophylaxis (PEP) following exposure to rabid or suspected rabies-infected animals.
Wound washing is an effective first-aid treatment against rabies. Wash all wounds and scratches immediately with soap or detergent and flush them thoroughly for about 5-10 minutes with water.
Seek immediate medical treatment with post-exposure prophylaxis, which will be given in accordance with the category of exposure. Immediately contact veterinary services or your animal health technician to assess the suspected rabid animal. Do not attempt to approach or capture the animal yourself.
Rabies disease in humans is diagnosed using PCR on saliva, cerebrospinal fluid and/or skin samples ante-mortem. Post–mortem investigations involve antigen testing of brain samples. More information on submission of samples and available tests are available from the disease index page on this website.